Weight loss surgery

Tomáš Paseka, MD
Weight Loss Surgery Department
Contacts and CV
Procedures
The surgery of obesity, so called bariatric surgery, weight reduction surgery or weight loss surgery (WLS), represents a series of various operations that have been employed in patients with morbid obesity that has failed to respond to previous conservative treatment or recurs with a yo-yo effect. The rationale for the operative treatment is based on the fact that the severe obesity significantly increases the health risks and shortens the life. The conservative therapy for obesity consisting of exercise, dietary and psychological treatment and pharmacotherapy, often achieves only a partial, and more importantly, only a temporary effect on the weight.
Classification of obesity is based on BMI (body mass index) which is calculated from weight (kg) and height (m). The BMI of a person = (his/her weight [kg]) / (his/her height [m2]). According to WHO obesity is classified in degrees: BMI of 30 and above means the 1st degree, BMI above 35 the 2nd degree and BMI above 40 the 3rd degree of obesity. Morbid obesity is labeled either BMI of 40 and above or in cases with severe health comorbidities also BMI of 35 and above.
What are the bariatric indication criteria?
According to internationally accepted guidelines the bariatric surgery is indicated only in morbid obesity keeping the primary goal to reduce its serious health risks under following following criteria:
- Morbid obesity, BMI 40 or more or BMI 35 and more in patients with comorbidities (e.g. type II diabetes, hypertension, hyperlipemia, metabolic syndrome, sleep apnea and joints and backbone overloading)
- Limit at SurGal Clinic is BMI 52
- Conservative treatment failure and/or insufficiency
- Consensual indication by the surgeon, obesitologist and psychologist
- Patient capable to stand an operation under general anaesthesia (lasting about 2 hours)
- No systemic disease
- No bulimia, serious psychiatric disease or abuse of drugs and/or alcohol
- The age of less than 60 years and no short life expectancy for any reason
- Presumption of a good and a smooth pre- and postoperative cooperation, compliance of the patient
What kind of bariatric operations have been in use ?
The most common operation are purely restrictive, limiting the gastric volume (as Gastric Banding, Gastric Sleeve Resection, Gastric curvate placation - WRAP). All the operations are performed under a general anesthesia at the operating theatre by means of minimally invasive surgery (laparoscopic surgery).
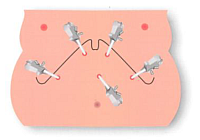
How is the laparoscopic surgery performed ?
Firstly the minimally invasive, laparoscopic approach requires an inflation of the peritoneal cavity by gas (CO2) through a special needle. The inflated belly gives enough of room for the surgeon to see and to manipulate the intraabdominal organs. Then more trocars, 5mm to 12 mm canulas are introduced through the abdominal wall. Through trocars special thin and long laparoscopic instruments are used which enables a miniinvasive performance of the whole operation. Then in all bariatric operations the left lobe of the liver has to be elevated to get an approach to the upper part of the stomach. Further technical details differ in each type of bariatric procedure. Extremely rarely, for example in huge fatty liver, when the laparoscopic procedure is not possible a 15 to 20 cm long incision has to be made to do the procedure in an open, traditional way.
The main technical steps in the Gastric banding surgery
In the most upper side of the stomach the pars flaccida of hepatogastric ligament is opened. On the opposite side of the stomach, at the top of the major curvature, the peritoneal adhesions close to Hiss angle are opened, too. Then with minimal possible tissue penetration a tunnel is created behind the posterior gastric wall by a blunt atraumatic and specialy curved instrument. This part of the operation with no direct visual control of the tip of the dissecting instrument requires the technical expertise of the surgeon. As soon as the stomach is encircled by an instrument a silicone gastric band is passed through the retrogastric “tunnel” and its ends are fixed together and locked to form a full ring compressing the upper end of the stomach. Few stitches are used to fix the band in the proper position and to avoid its postoperative slippage and dislocation. The peripheral end of the filling plastic tube is then pulled out of the belly and fixed to a special metal port that is fixed to thoracic fascia and stays hidden in the subcutaneous tissue. A drain is usually left for one or two days postoperatively to evacuate potential discharge from of the operated region. Gastric banding in various modifications has been used for nearly 30 years. It is the least invasive and the most frequently used bariatric method in Europe and Australia. The Laparoscopic adjustable gastric banding is a safe, reliable and well standardized minimally invasive procedure with long-lasting effect. Neither the stomach nor any other part of the gastrointestinal tract is cut, resected, shortened or open during the operation and the risk of complications is minimalised. The operation has purely restrictive effect with a unique advantage that it can be regulated, adjusted by gradual calibrated inflation of the hydraulic silicone system. Outpatient check ups and adjustments of the system are required few times a year.
The main principal of the operation is in the surrounding and encircling of the topmost part of the stomach by a silicon band which has an inflatable balloon at the side lying on the gastric wall. It is connected by a tube to a port which is located in the subcutaneous tissue at the chest wall, near the rib margin. We use products from famous producers (:Sweedish Adjustable Gastric Band/ SAGB from Ethicon Endo-Surgery, Johnson and Johnson Co. or
from Agency for Medical Innovation/ A.M.I.) which are designed to remain implanted for many years, although there is no “lifelong guarantee”. During the later postoperative course a special Huber needle enables a doctor to regulate the inner diameter of the band by inflating the hydraulic silicone system by isotonic saline solution. Probably nerves send signals to the brain about the pressure at the top of the stomach and this is recognized as a feeling of satiety soon after beginning of eating. This enables the patient to keep to a diet for a long time with no intractable hunger. The amount of food consumed reduces to half or even to one third of preoperative portions resulting in a weight reduction. It is important to take small mouthfuls of food and to chew carefully, since swallowing a large or insufficiently chewed mouthful may cause the food to become stuck above the band, causing regurgitation and discomfort.
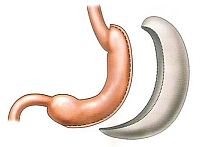
The main technical steps in the Gastric sleeve resection
First a thick gastric tube has to be placed into the stomach by the anaesthesiologist. Then the separation of the stomach and the surrounding tissue of greater omentum starts at the lower part of the stomach about 6-7 cm orally from the pylorus at the side of greater curvature. The opening the retrogastric space, the so called omental bursa, enables either a further sceletisation of the whole left margin of the stomach at the side of greater curvature or stapling of the stomach wall from the lower part of the stomach towards cardia in parallel to the gastric tube. The division of the stomach is made by serial shooting of special stapling cartridges of a laparoscopic stapler. Two lines of triple tiny iron staples close the stomach and cut it between both lines with no spillage of gastric content, no bleeding and no bacterial contamination of the peritoneal cavity. The major part of the stomach is finally removed from the abdominal cavity by a 4 -5 cm incision. A drain is usually left for one or two days postoperatively to evacuate potential discharge from of the operated region.
Gastric Sleeve Resection similarly to gastric band is a purely restrictive operation. The stomach is vertically transected and a tube is constructed from the gastric reservoir, reducing its capacity by about 60%. No foreign material is left in the body except staples and a major part of the stomach is removed, particularly the site of production of the hormone Ghrelin, responsible for feelings of hunger. The weight loss is usually quick within first months, usually lasts for two years, yet with no possibility of further adjustments and with no possibility of prolongation of the restrictive effect. The long term results of gastric sleeve resection (5 years and more) are not
known, yet, as this is a recently developed surgical technique.
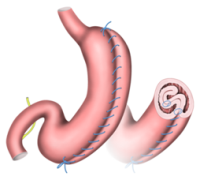
The main technical steps in the Gastric WRAP (greater curvate plication)
The surgery is performed in an operation theatre under general anaesthesia and lasts about 1 or 2 hours. The procedure involves insufflation of the abdominal cavity with CO2 under standardized, precisely determined conditions, which allows to insert an endoscopic camera and several long special operation tools through the abdominal wall with which it is possible to move aside the left liver lobe. Short gastric vessels are devided starting 5 cm from pylorus and continue along the greater gastric curvature up to the left diaphragmatic crus. After the fundus and gastric body are completely mobilised, the greater curvature is folded inward with 2 lines of suture to create a large intraluminal gastric fold. The gastric volume restriction is similar to sleeve gastrectomy but without any gastric resection. After the surgery, the usual procedure is to keep an abdominal drain for one day.
What preoperative procedures are needed?
Preoperative diet. A preoperative weight loss of at least half a stone 7lb (3 kg) within 2 – 3 weeks before the surgery is required as a significant contribution by the patient towards the smooth course of the laparoscopic operation. A strict reduction diet is necessary in order to diminish the liver and it should contain only 4.000 kJ [4MJ] (about 1000 Calories) of energy intake per a day comprising mainly from proteins (at least 50%). The diet should substantially limit any carbohydrates, sacharids (to only 25% - 30%) and should avoid any fat, lipids (to only 20%-25%). Lots of vitamins and unflavoured/unsweetened water are recommended.
Preoperative examinations. On the day of your admission to the hospital the following preoperative exams are on the schedule:
- laboratory test from your blood and urine
- abdominal ultrasound examination (sonography)
- lung and heart X-ray
- electrocardiography (ECG) alternatively with ergometry
- spirometry alternatively with complete pulmonary examination
- endoscopic examination of the stomach (gastroscopy)
- evaluation of your general health status by the internist specialist and by the anaesthesiologist.
- final preoperative consultation by the psychologist and the bariatric surgeon
What is the postoperative course like?
In laparoscopic surgery the postoperative recovery is short as the bodily pain from the abdominal wall is minor due to the absence of a long incision. Low doses of painkillers are usually sufficient. Also the inner organs start their work and recover sooner after laparoscopic procedure, which allows quick re-alimentation and an early discharge from hospital.
The first day after any weight loss surgery water and liquids are offered. Second day broth for lunch and dinner. Third day we offer yogurt or mashed food. Client is given dietary recommendations and is asked to follow all instructions written in there.
Usually one night after the operation is spent at the ICU, hospitalization at the ward lasts a further two days. The removal of stitches (10th to 20th day) could be done either by a family doctor (GP), at NHS Walk-in Centre or at the surgical outpatient department. You will be given a letter for your GP explaining him/her your surgery. Further check-ups (with optional adjustments in case of banding) are usually four times in the first year at postoperative months 3, 6, 9 and 12 , then twice a year for the next year and once a year thereafter for life.
What is the length of the hospitalisation?
The operation is scheduled to be performed by a minimally invasive approach, therefore if everything goes normally the discharge should be on the third postoperative day.
Are there any side effects?
A heartburn and other signs of gastro-oesophageal reflux may occur. The lifelong change in eating habits has to be accepted and kept, otherwise some deglutination problems may occur.
What are the most common complications in restrictive bariatric surgery?
The risk of an operation is lower than the risk of staying morbidly obese on a waiting list. Even in a very meticulous execution there may arise a complication during the operation or postoperatively. The most frequently cited are: Perioperative bleeding – can be usually controlled during the procedure by ultrasound hemostasis or electrocoagulation. In less than 1% transfusion or frozen plasma is required for blood substitution and improvement
of the hemostatic properties of the blood. Postoperative continuing or recurrent bleeding should be signalled by the abdominal drainage. In case of insufficiency of conservative treatment a reoperation may be required, yet extremely rarely.
Perforation of stomach, oesophagus or intestine is also an extremely rare complication. If recognised during the operation and repaired by a suture it has very good prognosis. If unrecognised early, it may cause a bacterial spillage of the peritoneal cavity with possible more serious consequences often requiring either an open or a laparosc opic re- operation.
Venous thrombosis and pulmonary embolism is a possible complication correlating with the length of the operation and immobilisation. Rarely it may emerge even if all recommended prophylactic measures are taken. Early postoperative physical activity and mobilisation on the first day are very important as a prophylactic measure. Superficial and dermal lesion – may emerge as a consequence of a heavy body, of a local compression or a local
reaction to disinfection solution and burn injury from short circuit of electric current.
Bacterial infection of the wound or of the foreign body is the most common complication that requires usually removal of the foreign material and prolonged local treatment with antibiotics and repeated change of the wound dressing.
If you have any further questions, don´t hesitate to contact us!
Your SurGal Clinic team