Total joints replacement - hip joint
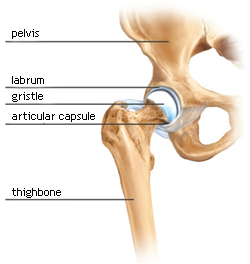
Anatomy
The hip joint is the spherical joint, in which the acetabulum and the head of the thighbone articulate. Contact surfaces of these bones are covered with hyaline gristle. The surface of the socket is formed by its bone part, the gristly labrum is mounted on its rim. The hip joint is statically stabilized by the strong articular capsule and dynamically by the muscular casing. The important muscles for standing and forward movement are especially the gluteal muscles, the iliopsoas and the hamstrings. There are important nerves running on the front and back side of the joint. There are vessels running on the front surface of the hip joint, supplying the whole lower limb.
Arthritis of the hip joint (coxarthrosis)
It is degenerative non-inflammatory affliction of hyaline gristle, showing itself first especially by pains during a movement and by acampsia. Later the pains arise in rest positions. Typical is also pain starting in the beginning of a movement and in the morning hours. Arthritis of the hip joint affects more than 10% of population.
Primary coxarthrosis – it rises under conditions of metabolic disorder of the gristle
Secondary coxarthrosis – the evocatory cause is not primarily on the metabolic base
The cause might be:
- development dysplasia of the joint
- rheumatoid arthritis, Bekhterev´s disease
- traumatogenic affliction, conditions after infectious complications
- conditions after aseptic necroses ( Perthes, corticosteroids)
X-ray picture can show arthritis as successive narrowing of the articulated joint and growth of fringe osteophytes, as subchondral sclerosis, sometimes even as creation of subchondral cystis with possibility of creation of bone necroses.
Arthritis is divided according to X-ray pictures to four stages according to Kellgren and Lawrence (1957):
- I. stage: medial narrowing of the articulated joint, beginning of creation of osteophytes
- II. stage: certain inferomedial reduction of the articulated joint, obvious osteophytes
- III. stage: the articulated joint is distinctively narrowed, sclerotic changes of detritus cystis, deformation of the head shape as well as acetabula
- IV. stage: disappearing of the articulated joint with scleroses and cystis, advanced deformation
Coxarthrosis therapy
There are mainly pharmacological and rehabilitative procedures used during the early stages of coxarthrosis. Modification of sport activities is really important. Suitable sport activities are cycling and swimming. It is essential to maintain optimal weight of a patient to prevent bearing joints overloading. Recommended medication particularly consists of non steroidal antiflogistics.
During more advanced stages of coxarthrosis it is important to estimate clinical condition and consider possibility of saving surgical practices. It is suitable to use arthroscopic therapy of femoroacetabular impingement (syndrome of shocks around osteophytes), eventually osteotomy of the upper end of the thighbone.
During advanced stage of caxarthrosis is often necessary to undertake the implantation of the hip replacement (total endoprosthesis - TEP).
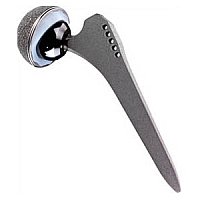
Hip replacement - Alloplastic – Total endoprosthesis (TEP)
Alloplastic of the hip joint is a replacement of a deformed joint with a surgical implant. The socket of acetabula, as well as the head of the thighbone are replaced.
Cemented endoprosthesis:
- polyethylene socket fixed with bone cement
- stem fixed with bone cement
Hybrid endoprosthesis:
- socket not cemented – usually from titan
- stem fixed with bone cement
Non cemented endoprosthesis:
- non cemented socket
- non cemented stem
There is a filler put into imbedded socket. It makes sliding surface, the head of endoprosthesis is mounted on the stem cone. The sliding surfaces are made with materials like CrMoCo steel, polyethylene, ceramics and oxinium.
Preoperative preparation
It is necessary that a patient undertakes thorough preoperative examination. In our Grand Class Ambulance we perform standard preoperative examination (EKG, laboratory examination, X-ray of the heart and lungs), dental examination, gynaecological and urological examination. During the preoperative period is needed to regulate medication of the drugs, influencing blood coagulation. A patient gets axillar crutches and medication to prevent toxic epidermal necrolysis.
Surgery
The time spent by a patient in a chart room is about 120 min. The patient is always guided by a physician anaesthetist and a nurse anaesthetist. In most of the cases it is suitable to perform the alloplastic of the hip joint under spinal anaesthesia, so the patient is conscious during the surgery. Only the operated limb is insensible. To evoke pleasant atmosphere patients are given sedatives and they can listen to their favourite music during the surgery. The surgery itself takes approximately 90 min. To replace the lost blood it is used recuperation, the blood sucked from the wound is returned back to the blood circulation after special treatment. It is not often necessary to transfer blood of another person or to perform auto transfusion.
Postoperative treatment
A patient goes from the chart room to the postoperative department (Intensive Care Unit), where his/her state is monitored for approximately 24 hours. Further treatment then usually takes place on standard and extra beds of our institution. During after-treatment stay the patient is visited by experienced physiotherapist who leads the rehabilitation. Within one week patients are mostly so mobile and independent that they can be transferred to another place. Stitches removing is recommended on the 12. – 14. day of the after-treatment. Patients visit our ambulance for regular check-ups in the 1, 3, 6, 12 month after the surgery. In the period of one year they can choose sequential therapy in a health-resort. Subsequently they are regularly observed every year.
Complications and risks
Complications can arise after every surgery, still they are successfully reduced to minimum through modern techniques and materials and high specialization of the physicians.
The most common complication of alloplastic of the hip joint is secondary healing and longer time taking serosal wound ooze. In most of the cases it is enough to rebind the wound regularly, eventually to dose antibiotics. If the inflammatory parameters rise in the cultivated infectious agent, it is sometimes necessary to undertake a corrective surgery of the joint and eliminate the infection.
The dislocation of TEP happens especially in the period of 6 weeks after the implantation of TEP. In this period the soft tissues are not adequately healed. Therefore patients are during after-treatment thoroughly informed on positions they should avoid in the early postoperative period.